Reading Brain MRIs
What and why you should know about this
Brain MRI is one of the most annoying things on Earth. I guarantee that the first time you set your eyes on an MRI scan, you simply don't know what to do with it. Number 1, the anatomy is sophisticated - one has to be really sure of where the structures are and what they translate functionally (for instance, a lesion over the frontal lobe affects motor activity); Number 2, there is no 'the' MRI Scan. There are loads of sequences. To name a few, as I work with stroke images, I have to deal with structural scans (i.e. those which deal with the actual brain) involving 4 sequences, and vascular scans.
So, where should we start?
VERY-BRIEF INTRODUCTION
What the heck is MRI?
A physicist, or medical engineer, might give you a 100-page thesis on what MRI entails and its history. I'm no physicist, nor am I a radiographer. I'm just a bumblebee struggling to survive.
MRI is the 'best' type of imaging available (best is in quotes since it's a very vague concept). It shows the clearest of details and uses a magnetic field so it doesn't carry any ounce of radiation. Look at CT and X-Ray and you'll know what I'm talking about. MRI works best when visualising soft tissue structures (for bone, CT and X-Ray are better).
REASONS TO KNOW
Like, how is it going to affect me?
For starters, it is a great deal. Knowing how to read Brain MRI Scans is not a skill essential only to radiologists and neurologists. Medicine is a multi-disciplinary subject and pathologies often traverse traditional boundaries of human understanding. Even if a patient presents with a non-neurological issue, such skills will eventually come in handy. True story, I've once seen a patient who started off with Stage 4 prostate cancer and presented with a scalp mass. It was quite sobering the first time I saw it- the team immediately did a CT Scan to check whether it was intra-cranial or extra-cranial. This is a huge deal, since prostate cancer is osteoblastic, meaning that its bone metastases lead to an increase in bone density. Metastasising to the skull is totally possible. Moreover, due to the nature of the cancer (metastatic), haematological spread was imminent. Metastasising to the brain is definitely an alarming possibility and poses more problems than a skull metastasis. One can die from a brain metastasis due to the risk of brain herniation.
CT is the most common first-line modality when you're dealing with patients with brain pathologies. MRI is kind of a commodity - it's hard to get. However, emergency physicians at least need to know the value of MRI. This is no better exhibited in patients presenting with transient ischaemic attacks (TIA) and stroke. They happen spontaneously and often show nothing on the initial CT, depending on the stage of the infarct. MRI evaluation is required. For more details, refer to González et al (2013) [1]. Even when it comes to evaluating CT Scans, learning how to read MRI entails the acquisition of transferable skills which are going to be invaluable, e.g. recognition of anatomical structures, basic principles of imaging. The last thing you want to do is to fail to recognise the main signs of a serious pathology like stroke. Well, not trying to scare anyone, but a junior doctor (I witnessed with my own eyes) got chastised by the consultant for not being able to see the subtle loss of insular ribbon which is the early sign of an infarct.
Finally, it's fun! I can't tell you how much I enjoyed reading them (by the end of the data collection stage) - there's a steep learning curve but you do derive immense satisfaction from the fact that you actually understand what the hell goes on. The milestone of my achievement was recognising and remembering all 7 segments of the internal carotid artery (Bouthillier Classification). [2]
I realise that it's totally impossible to encapsulate everything on a single webpage. So, I've decided to give you all an outline of the most crucial Brain MRI sequences (both structural and vascular scans) and a run-through of a stroke case to illustrate my way of dealing with it.
For more details through your learning (trust me, the learning curve is very steep), consult Radiopaedia.
Reference List:
[1] González RG, Copen WA, Schaefer PW, et al. (2013). The Massachusetts General Hospital acute stroke imaging algorithm: an experience and evidence based approach
Journal of NeuroInterventional Surgery;5:i7-i12.
[2] Bouthillier A., van Loveren H., & Keller J. (1996). Segments of the Internal Carotid Artery: A New Classification. Neurosurgery, 38(3), 425-433. https://doi.org/10.1097/00006123-199603000-00001

MRI Sequences (Crucial Ones)
The most important ones and what they're about are listed below:
1. T1-weighted imaging - lights up when there is fat, e.g. tumour; also lights up when there is subacute haemorrhage;
2. T2-weighted imaging - lights up when there is water, e.g. cerebrospinal fluid over the ventricles; usually confusing;
3. FLAIR - also T2-weighted but the fluid signal over the ventricles is suppressed, so that we can spot pathologies in the brain tissue; excellent for white matter hyperintensities and perivascular spaces, both being signs for small vessel disease;
4. Diffusion-Weighted Imaging (DWI) - possibly 'the one' for stroke, as it shows restriction in the diffusion of water molecules. This is usually significant since in stroke due to cytotoxic oedema (where water flows into the cells leading to gross swelling).
5. MRA (MR Angiography) - visualising vascular characteristics, including anatomy, stenoses and occlusions.
Other noteworthy ones (but not important enough to be elaborated) include Gradient Echo, Susceptibility-weighted imaging (SWI) and ADC (Apparent Diffusion Coefficient).
For the clever clogs out there who want to know more, refer to the following journal article:
Bitar R, Leung G, Perng R, et al. (2006). MR Pulse Sequences: What Every Radiologist Wants to Know but Is Afraid to Ask. Radiographics, 26(2), 513-537. https://doi.org/10.1148/rg.262055063
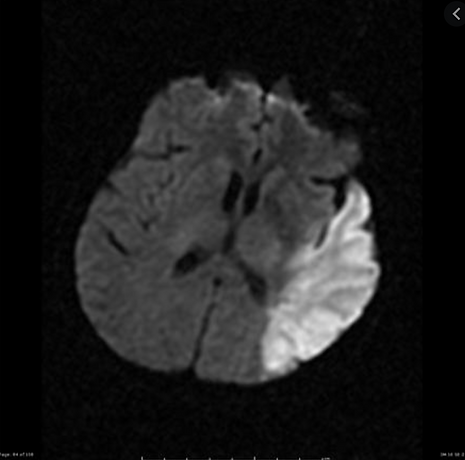
Case Study - Acute Ischaemic Stroke (Refer to image below)
To make life much simpler, I am only going to show you my general approach and what other things I also do apart from reading this image (sorry if the quality isn't that good - I've got it from my phone archive...)
1. What image modality is this? MRI.
2. What sequence is this? DWI (don't worry - hospital records have them labelled; immediate identification comes with practice and experience).
3. What looks weird? Lesion over the Left (X Right!!! In radiology, almost everything's flipped).
4. Why does it look weird? Higher intensity (MRI = intensity; CT = density) than surrounding brain tissue.
5. What can it mean? Diffusion restriction --> ischaemic stroke? Confirm with clinical records. Read with context.
6. What structures does it encompass? Left Parietal, Temporal and Occipital Lobes (although occipital lobe involvement is minimal).
7. What is the size of the lesion? Measure with the ruler function on the hospital computer.
8. Are there any other lesions? What about the other side? No. There is only one lesion. The brain is asymmetrical.
9. As you think it's a stroke, what else should you check? Vascular involvement. In this case, the left Middle Cerebral Artery (MCA) is affected.
10. (advanced) Alright, can you tell me which segment(s) is/are affected? As the left basal ganglia are spared, M1 is not affected (M1 gives lateral lenticulostriate perforators which supply the basal ganglia). The infarct is likely to be resultant from the severe narrowing/occlusion of M2 and beyond.
11. Is that it? Are you confident? (from real-life professor...I've seen things...)
No, I'm not confident. I want to review other images in the stack and check if there are lesions elsewhere, particularly in the MCA territory. I want to check previous records to see about the evolution of the lesion. I also want to check other sequences (including FLAIR and ADC) to confirm that it's not a mere artefact (aka pseudo-pathology, one of the ways MRI trips you up).